", treatment yellow jacket sting".
By: E. Aschnu, M.S., Ph.D.
Professor, University of South Carolina School of Medicine
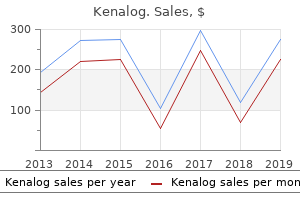
Pleural inflammation is associated with pain that worsens with deep breathing medications that cause weight gain , limiting full lung expansion medicine list . Pleuritic pain may resolve as pleural fluid increases because contact between the irritated pleural membranes is reduced medications given to newborns . In general medications quizzes for nurses , a minimum of approximately 400 mL of pleural liquid is required for roentgenographic visualization in upright views of the chest. When effusion is moderate, chest radiographs demonstrate uniform water density and widened interspaces on the affected side, with displacement of the mediastinum to the contralateral hemithorax. In acutely ill children, when only a supine view is available, detection of pleural fluid is problematic. Generalized haziness of the affected hemithorax or accentuated pleural reflection may be the only clue to this disorder. Standard posteroanterior chest radiographs may be inadequate to fully evaluate pleural fluid. Lateral decubitus radiographs provide valuable information about the quantity and quality of effusions, allow evaluation of the underlying parenchyma, and assist in planning investigations and therapy. Thin, mobile (nonloculated) pleural fluid will layer out on the dependent side. Lateral decubitus views with the unaffected side inferior may enhance visualization of the underlying parenchyma on the affected hemithorax. Posteroanterior chest radiograph demonstrating lung hyper- inflation and perihilar interstitial infiltrates, consistent with Mycoplasma pneumonia. Anteroposterior supine chest radiograph with pleural fluid evident between the chest wall and the lung (arrow). Note the generalized increased haziness of the right hemithorax caused by the accumulation of pleural fluid. Posteroanterior erect chest radio- graph demonstrating bilateral pleural effusions, with the effusion on the left greater than that on the right. Also evident are atelectasis in the right upper lobe and consolidation in the left lower lobe. Air and Liquid in the Pleural Space 981 Chapter 70 dent, obtained in the same patient as in Figure 70-5, confirming the presence of a free-flowing right pleural effusion. Left lateral decubitus chest radiograph showing the layering of a nonloculated left pleural effusion. As little as 50 mL of pleural liquid can be detected with properly exposed lateral decubitus views; this liquid is seen as a layering of liquid density in the dependent portion of the thoracic cavity. Moreover, a decubitus film demonstrating more than 10 mm of pleural fluid between the inside of the chest wall and the lung indicates an effusion of sufficient volume for thoracentesis. Failure of the liquid to shift from the upright to the decubitus view indicates loculation, as commonly seen in staphylococcal empyema. Evaluation of the parenchyma and differentiation of loculated effusion caused by pleural fibrosis or infiltration may require adjunctive imaging modalities. Upright chest radiograph of a child with nephrotic syndrome, demonstrating right infrapulmonary pleural effusion. The right hemidiaphragm shows peak elevation laterally (arrow) and relative lucency of the costophrenic sinus, which are signs that indicate an intrapulmonary location of the liquid. A loculated parapneumonic effusion is differentiated from a lung abscess by the angle made between the fluidfilled mass and the chest wall. An empyema usually creates an obtuse angle where it meets the chest wall, in contrast to the acute angle produced by an abscess. Further thoracic imaging techniques are required to demonstrate bronchopleural fistulas. Radiopaque contrast material is injected into the affected pleural space through a needle or an existing chest tube. As the patient coughs, the contrast material opacifies the fistula and spreads throughout the bronchial tree.
The half-life of erythrocytes is quite long (120 days) treatment goals and objectives , so that erythrocyte zinc concentrations will not reflect recent changes in body zinc stores medications by mail . Age-related changes in erythrocyte zinc in infants and children (Nishi nioxin scalp treatment , 1980) and adolescent females have been reported (Kenney et al treatment 21 hydroxylase deficiency . Leukocytes Leukocytes have a shorter half-life than erythrocytes and should therefore reflect changes in zinc status over a shorter time-period. Relatively large volumes of blood are required, and isolation of the leukocytes and their subsequent analysis is lengthy and technically difficult, limiting the use of these indices, especially for infants and young children. Changes in the relative proportions of leukocyte subsets with physiological state. Finally, comparison of results between different studies is difficult because no consensus exists as to how to express zinc concentrations in the cell types (Thompson, 1991). Urine Depletion of body zinc stores causes a reduction in urinary zinc excretion (Hess et al. Supplementation with high (100 mg) but not moderate (50 mg) zinc intakes increases urinary zinc excretion (Verus & Samman, 1994). Several factors can affect urinary zinc concentrations, however, making interpretation of the results difficult. Hyperzincuria is also present in disorders such as cirrhosis of the liver and diabetes mellitus, after injury, burns and acute starvation, in certain renal diseases and infections, and after treatment with chlorothiazide. Hypertensive patients on long-term therapy with chlorothiazide may therefore be vulnerable to zinc deficiency (Prasad, 1983). The measurement of zinc in urine is therefore helpful for diagnosing zinc deficiency only in apparently healthy persons. In general, 24-h urine collections are preferred because diurnal variation in urinary zinc excretion occurs. Hair the use of hair zinc concentrations as an index of zinc status has been controversial (Hambidge, 1982). Available evidence suggests that low zinc concentrations in hair samples collected during infancy and childhood probably reflect a chronic suboptimal zinc status when the confounding effect of severe protein-energy malnutrition is absent (Hambidge et al. Hair zinc cannot be used in cases of very severe malnutrition and/or severe zinc deficiency, when the rate of growth of the hair shaft is often diminished. Low hair zinc concentrations have been reported in infants and children with impaired linear growth (Hambidge et al. Moreover, in some of these studies, the low hair zinc concentrations have been related to low availability of dietary zinc (MacDonald et al. In some but not all of these cases of suboptimal zinc status, hair zinc concentrations have increased in response to zinc supplementation. The discrepancies may arise from variations in the dose, duration of zinc supplementation, and confounding effects of season on hair zinc concentrations. Periods of 6 weeks or less are 112 Kinetics and Metabolism in Mammals probably too short for a response, since hair zinc reflects only chronic changes in zinc status (Greger & Geissler, 1978; Lane et al. Unfortunately, when studies are made over a longer term, seasonal changes in hair zinc concentrations must also be taken into account when interpreting the results (Hambidge et al. Standardized procedures for sampling, washing and analysing hair samples are essential in all studies. Variations in hair zinc concentrations with hair colour, hair beauty treatments, season, sex, age, anatomical site of sampling (scalp or pubic), and rate of hair growth have been described (Hambidge, 1982; Taylor, 1986; Klevay, 1987; Gibson et al. The effects of these possible confounding factors must be considered in the interpretation of hair zinc concentrations. Many investigators have failed to find any positive correlations between the zinc content of hair and serum/plasma zinc concentrations (Klevay, 1970; Lane et al. The zinc content of the hair shaft reflects the quantity of zinc available to the hair follicles over an earlier time interval. Positive correlations between hair zinc concentrations and serum zinc are only observed in chronic, severe zinc deficiency in the absence of confounding factors. The validity of hair zinc as a chronic index of suboptimal zinc status in adults is less certain, and further studies are required. Saliva Zinc concentrations in mixed saliva, parotid saliva, salivary sediment and salivary supernatant have all been investigated, but their use as indices of zinc status is equivocal (Greger & Sickles, 1979; Freeland-Graves et al. Alternatively, physiological functions dependent on zinc, such as growth, taste acuity and immune competence, can be assessed.
. HIV Symptoms in Men After 6 Months.
Some acoustic characteristics of cough are quite specific for certain diseases treatment for vertigo , such as the sound of a barking seal in viral croup or the whooping noise in pertussis medicine 91360 . In patients with chronic cough medications for bipolar disorder , the physician should weigh the possible causes in view of their prevalence at different ages (Table 8-2) medicine pictures . Also, complications of severe coughing paroxysms, such as pneumothorax, cough syncope, or nonsyncopal neurologic manifestations, should be considered. Regarding the last, the physician should inquire about lightheadedness, headache, visual disturbance, paresthesia, and tremor. This noise may be a nonmusical hiss, much like the one produced in normal subjects at increased rates of ventilation, or it may have the musical qualities of stridor and snoring. Also, bubbling and crackling noises may be heard, and the tactile perception may contribute to the impression of a "rattly" chest in these patients. The physician should focus attention on the noisegenerating structures of the extrathoracic airways that are located at points of anatomic narrowing. The most common cause of noisy breathing in toddlers and young children is nasopharyngeal obstruction; in young infants, laryngomalacia is a leading cause. Placing the stethoscope within the airstream in front of the mouth, one hears predominantly those sounds that are produced locally in the mouth and larynx. Noisy breathing is a common finding in patients with asthma and bronchitis and does not necessarily reflect intrathoracic airway pathology because the upper airways are also frequently affected in these patients. To clarify the causes of noisy breathing, the parents or patient should describe their own perceptions of the noise: Does it occur during inspiration, expiration, or both? Is it just an exaggeration of the normal breath sound noise, or does it have musical qualities? The physician should also inquire about associated cough, sputum production, and dyspnea. Children may suffer from partial obstruction of the upper airways during sleep; complete obstruction, which is found in adult patients with sleep apnea, is less common. The physician should inquire about the typical signs and symptoms found in patients with increased work of breathing and abnormal sleep patterns at night (Box 8-1). In the older child and adolescent, the physician should first inspect the nasal passageways and proceed to an examination of the oropharynx before auscultation of the neck and thorax. The acoustic signs should be checked while the patient breathes first with the mouth open, and then closed. In younger children, examination of the nose and mouth is unpopular and often results in agitation and crying. Noisy breathers should be examined when they are sitting or standing upright and when they are lying down because upper airway geometry is position dependent and may influence the respiratory sounds. The examiner should also note abnormal crying or speech in the patient, as this may point to laryngeal disease. Essentially, it is a very loud inspiratory wheeze originating from extrathoracic airways. When asking the patient or the parents about wheezing and stridor, one should keep in mind that the use of lung sound terminology among nonprofessionals is not better standardized than it is among health care providers. Therefore, the physician should inquire about musical, whistling noises during respiration, and, if necessary, demonstrate stridor or the forced expiratory wheeze that can be produced even by healthy individuals. Most typically, wheezing is associated with hyperreactive airway disease, but any critical narrowing of the airways can produce wheezing. Box 8-2 lists conditions other than asthma that may be associated with wheezing and stridor. The wheezing that is typical in asthma originates from oscillations of airways at many sites. Obstruction of a single airway can produce a single monophonic wheeze or, in the obstruction of extrathoracic airways, stridor. Both inspiratory and expiratory wheezes are present in the majority of asthmatic patients. The audible expiratory phase (expirium) is typically prolonged because of wheezing. Objectively measured expiratory time (expiration), however, is rarely prolonged except in very severe airway obstruction. Respiration becomes ominously silent, and the patient may have carbon dioxide retention and cyanosis.
The greater the component of Pdif that is incorporated into the Rint measurement treatment trends , the higher Rint will be with respect to pure Raw and the more it will approach the resistance of the total respiratory system shinee symptoms mp3 . Even when Pm is linearly back-extrapolated to the beginning of the interruption treatment for piles , it is still partially dependent on the final part of the pressure-time curve medications diabetic neuropathy . Reference equations derived from over 1000 young children (ages 3 to 13 years) have recently been collated to provide sex-specific reference equations for Rint. Actual pressure-time trace showing mouth pressure (Pm) during a 100-msec interruption. The straight line represents the linear back-extrapolation of Pm to the beginning of the interruption (T0 when Pm reaches 25% of the difference between the first peak and the baseline value) using pressures measured 30 msec and 70 msec later. Technically acceptable interruption for assess- 0 30 Time (msec) 60 Pulmonary Function Tests in Infants and Preschool Children 2. Sex-specific reference equations for expiratory interrupter resistance (Rinte; solid line) expressed as kPa. The major limitation is that it is dependent on rapid equilibration between mouth pressure and alveolar pressure after interruption. Ventilation inhomogeneity or severe bronchial obstruction, as well as compliance of the cheeks and upper airways, may delay this equilibration, such that alveolar pressure and hence Rint will be underestimated. This has led to some concerns about using Rint as an outcome measure in challenge 192 General Clinical Considerations tests. Furthermore, there is still some controversy about the best way to calculate and report results, particularly with respect to how to calculate pressure at the moment of interruption. The role of Rint as the primary outcome in challenge tests and the usefulness of the interrupter technique in comparison with other techniques for lung function testing in preschool children remain to be determined. Data are usually collected over periods of 8 to 16 seconds, with up to five technically satisfactory sets being recorded for each child. Respiratory impedance (Zrs) is calculated by distinguishing the changes in pressure and flow caused by the applied oscillations from those occurring during tidal breathing. The superimposed pressure oscillations during normal spontaneous breathing are composed of several frequencies, allowing assessment of Rrs and Xrs at several frequencies simultaneously by Fast Fourier analysis. Since all frequencies are applied in just one rectangular pulse, the measurement time is reduced while maintaining a very low noise-signal ratio. The upper limit is dictated by possible artifacts related to compliance of the cheeks and pharyngeal wall, which may result in considerable upper airway wall vibration if respiratory impedance is measured at high frequencies, especially in small children. The head generator technique was designed to minimize upper airway wall motion, but it requires more cumbersome equipment than the standard technique and is now rarely used. It can also be used to define impedance of the lungs in infants and older subjects, but since this requires an esophageal catheter to measure transpulmonary pressure, measurements in preschool children are generally limited to respiratory system impedance, with trans-respiratory pressure changes being measured at the mouth (Pm). The impedance of the respiratory system (Zrs) can be measured by superimposing small-amplitude pressure oscillations on the respiratory system and measuring the resultant oscillatory flow. B, Pressure oscillations are applied either at the airway opening using a standard generator or around the entire head (head generator). The latter method is more cumbersome, but may reduce artifacts due to the compliance of the upper airway, which may be particularly important in young children. Nevertheless, there are marked differences between these equations, including much higher values obtained when using a modified facemask rather than a mouthpiece, reflecting the wide range of techniques used. Currently the wide degree of variability between healthy children of similar age or body size limits the extent to which this technique can be used to assess either the presence or the severity of airway disease within individuals. It may, however, be a valuable tool for detecting changes within individuals on the same occasion, particularly when assessing bronchial responsiveness. Methods of assessing respiratory muscle strength include determination of maximal inspired and expired pressure during respiratory efforts against brief airway occlusion. Consequently, work is being undertaken to evaluate the discriminative ability of alternative indices, such as the tension-time index of the respiratory muscles. Although still to be evaluated in infants and young children, the latter has several advantages in that it is noninvasive, does not require placement of gastric or esophageal pressure transducers, and assesses muscle fatigue in all of the respiratory muscles, not simply the diaphragm. A recent modification, using magnetic rather than electrical 194 General Clinical Considerations Time-based recording of flow and pressure Pressure (cm H2O) Flow (L/sec) 2 1 0 1 2 2 1 0 1 2 0 2 4 6 Time (sec) Signals transformed to the frequency domain 0. Despite earlier convictions that reliable spirometric measurements could not be routinely obtained in children younger than 6 years of age, the majority of preschool children are able to perform satisfactory maneuvers, provided suitable modifications are implemented, as discussed in the following sections.