"Cheap 1 mg arimidex otc, breast cancer 80s".
By: M. Dawson, M.B. B.CH. B.A.O., Ph.D.
Associate Professor, University of South Carolina School of Medicine Greenville
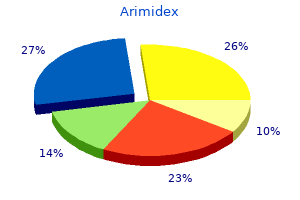
Tissue from any ulcer of the oral cavity that does not heal in 2 weeks should be examined through biopsy women's health clinic omaha ne order generic arimidex on line. As the cancer progresses zithromax menstrual cycle order arimidex with visa, the patient may complain of tenderness; difficulty in chewing menopause journal article arimidex 1mg, swallowing womens health garcinia cambogia article discount 1mg arimidex overnight delivery, or speaking; coughing of blood-tinged sputum; or enlarged cervical lymph nodes. Diagnosis is based on the health history and physical examination and the results of fine needle aspiration biopsy. Management of salivary gland tumors evokes controversy, but the common procedure involves partial excision of the gland, along with all of the tumor and a wide margin of surrounding tissue. Dissection is carefully performed to preserve the seventh cranial nerve (facial nerve), although it may not be possible to preserve the nerve if the tumor is extensive. Radiation therapy alone may be a treatment choice for tumors that are thought to be contained or if there is risk of facial nerve damage from surgical intervention. Local recurrences are common, and the recurrent growth usually is more aggressive than the original. It has also been observed that patients with salivary gland tumors have an increased incidence of second primary cancers (Bull, 2001). Assessment and Diagnostic Findings Diagnostic evaluation consists of an oral examination as well as an assessment of the cervical lymph nodes to detect possible metastases. Biopsies are performed on suspicious lesions (those that have not healed in 2 weeks). High-risk areas include the buccal mucosa and gingiva for people who use snuff or smoke cigars or pipes. For those who smoke cigarettes and drink alcohol, high-risk areas include the floor of the mouth, the ventrolateral tongue, and the soft palate complex (soft palate, anterior and posterior tonsillar area, uvula, and the area behind the molar and tongue junction). Medical Management Management varies with the nature of the lesion, the preference of the physician, and patient choice. Surgical resection, radiation therapy, chemotherapy, or a combination of these therapies may be effective. In cancer of the lip, small lesions are usually excised liberally; larger lesions involving more than one third of the lip may be more appropriately treated by radiation therapy because of superior cosmetic results. The choice depends on the extent of the lesion and what is necessary to cure the patient while preserving the best appearance. Cancer of the tongue may be treated with radiation therapy and chemotherapy to preserve organ function and maintain quality of life. A combination of radioactive interstitial implants (surgical implantation of a radioactive source into the tissue adjacent to or at the tumor site) and external beam radiation may be used. If the cancer has spread to the lymph nodes, the surgeon may perform a neck dissection. Surgical treatments leave a less functional tongue; surgical procedures include hemiglossectomy (surgical removal of half of the tongue) and total glossectomy (removal of the tongue). Often cancer of the oral cavity has metastasized through the extensive lymphatic channel in the neck region. The combination of alcohol and tobacco seems to have a synergistic carcinogenic effect. About 95% of cases of oral cancer occur in people older than 40 years of age, but the incidence is increasing in men younger than age 30 because of the use of smokeless tobacco, especially snuff (Centers for Disease Control and Prevention, 2002). Cancer of the oral cavity accounts for less than 2% of all cancer deaths in the United States. Men are afflicted more often than women; however, the incidence of oral cancer in women is increasing, possibly because they use tobacco and alcohol more frequently than they did in the past. The 5-year survival rate for cancer of the oral cavity and pharynx is 55% for whites and 33% for African Americans. Of the 7400 annual deaths from oral cancer, the distribution by site is estimated as follows: tongue, 1700; mouth, 2000; pharynx, 2100; other, 1600 (American Cancer Society, Cancer Facts and Figures, 2002). For more information about dentures, see the accompanying Gerontologic Considerations box. Both the internal and the external structures of the mouth and throat are inspected and palpated. Dentures and partial plates are removed to ensure a thorough inspection of the mouth. In general, the examination can be accomplished by using a bright light source (penlight) and a tongue depressor. The patient is instructed to open the mouth wide; a tongue blade is then inserted to expose the buccal mucosa for an assessment of color and lesions.
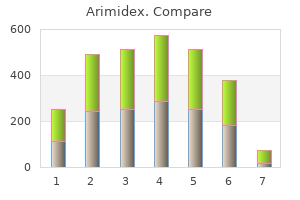
Diet It is not unusual for patients undergoing thoracotomy to have poor nutritional status before surgery because of dyspnea menopause at 80 generic 1mg arimidex with amex, sputum production menopause test buy generic arimidex 1mg online, and poor appetite menstrual sea sponge order arimidex 1mg fast delivery. Dyspnea pregnancy mode cheap arimidex line, restlessness, increasing respiratory rate, increasing blood pressure, and tachycardia are warning signs of impending respiratory insufficiency. Pulse oximetry is used to monitor oxygenation and to differentiate causes of restlessness. A B C D E F (A) Hold hand of the affected side with the other hand, palms facing in. Press down on hands, consciously pulling the abdomen in and stretching up from the waist. Hold this position a moment, and begin exhaling while lowering the body slowly to the original position. A liquid diet is provided as soon as bowel sounds return; the patient is progressed to a full diet as soon as possible. Small, frequent meals are better tolerated and are crucial to the recovery and maintenance of lung function. In addition, the nurse monitors the patient at regular intervals for signs of respiratory distress or developing respiratory failure, dysrhythmias, bronchopleural fistula, hemorrhage and shock, atelectasis, and pulmonary infection. Respiratory distress is treated by identifying and eliminating its cause while providing supplemental oxygen. If the patient progresses to respiratory failure, intubation and mechanical ventilation are necessary, eventually requiring weaning. Dysrhythmias are often related to the effects of hypoxia or the surgical procedure. Pulmonary infec- tions or effusion, often preceded by atelectasis, may occur a few days into the postoperative course. Pneumothorax may occur following thoracic surgery if there is an air leak from the surgical site to the pleural cavity or from the pleural cavity to the environment. Failure of the chest drainage system will prevent return of negative pressure in the pleural cavity and result in pneumothorax. The nurse maintains the chest drainage system and monitors the patient for signs and symptoms of pneumothorax: increasing shortness of breath, tachycardia, increased respiratory rate, and increasing respiratory distress. Bronchopleural fistula is a serious but rare complication preventing the return of negative intrathoracic pressure and lung reexpansion. Depending on its severity, it is treated with closed chest drainage, mechanical ventilation, and possibly talc pleurodesis (described in Chap. Hemorrhage and shock are managed by treating the underlying cause, whether by reoperation or by administration of blood products or fluids. The early symptoms are dys- Chapter 25 pnea, crackles, bubbling sounds in the chest, tachycardia, and pink, frothy sputum. The recovery process may be longer than the patient had expected, and providing support to the patient is an important task for the home care nurse. Because of shorter hospital stays, attending follow-up physician appointments is essential. The nurse teaches the patient about the importance of keeping follow-up appointments and completing laboratory tests as prescribed to assist the physician in evaluating recovery. The home care nurse provides continuous encouragement and education to the patient and family during the process. As recovery progresses, the nurse also reminds the patient and family about the importance of participating in health promotion activities and recommended health screening. Demonstrates improved gas exchange, as reflected in arterial blood gas measurements, breathing exercises, and use of incentive spirometry 2. Shows improved airway clearance, as evidenced by deep, controlled coughing and clear breath sounds or decreased presence of adventitious sounds 3. Has decreased pain and discomfort by splinting incision during coughing and increasing activity level 4. Shows improved mobility of shoulder and arm; demonstrates arm and shoulder exercises to relieve stiffening 5. Exhibits less anxiety by using appropriate coping skills, and demonstrates a basic understanding of technology used in care 7. Is free of complications, as evidenced by normal vital signs and temperature, improved arterial blood gas measurements, clear lung sounds, and adequate respiratory function For a detailed plan of nursing care for the patient who has had a thoracotomy, see the Plan of Nursing Care.
Cheap arimidex online master card. 30 Min Low Impact Cardio Workout for Beginners - HIIT Beginner Workout Routine at Home for Women Men.
The infection usually causes deformity of the valve leaflets sepia 9ch menopause cheap 1 mg arimidex fast delivery, but it may affect other cardiac structures such as the chordae tendineae menstrual uterine contractions purchase arimidex 1mg otc. Patients at higher risk for infective endocarditis are those with prosthetic heart valves menopause 8 months no period buy cheapest arimidex and arimidex, a history of endocarditis womens health zumba discount arimidex 1 mg without a prescription, complex cyanotic congenital malformations, and systemic or pulmonary shunts or conduits that were surgically constructed (eg, saphenous vein grafts, internal mammary artery grafts). At high risk are patients with rheumatic heart disease or mitral valve prolapse and those who have prosthetic heart valves (Chart 29-2). Hospital-acquired endocarditis occurs most often in patients with debilitating disease, those with indwelling catheters, and those receiving prolonged intravenous or antibiotic therapy. Patients receiving immunosuppressive medications or corticosteroids may develop fungal endocarditis. Chapter 29 Management of Patients With Structural, Infectious, and Inflammatory Cardiac Disorders 781 as well. A definitive diagnosis is made when a microorganism is found in two separate blood cultures, in a vegetation, or in an abscess. Three sets of blood cultures (with each set including one aerobic and one anaerobic culture) should be obtained before administration of any antimicrobial agents. Negative blood cultures do not totally rule out the diagnosis of infective endocarditis. An echocardiogram may assist in the diagnosis by demonstrating a moving mass on the valve, prosthetic valve, or supporting structures and by identification of vegetations, abscesses, new prosthetic valve dehiscence, or new regurgitation (Braunwald et al. All catheters are removed as soon as they are no longer needed or no longer function. Complications Even if the patient responds to the therapy, endocarditis can be destructive to the heart and other organs. Heart failure and cerebral vascular complications, such as stroke, may occur before, during, or after therapy. The development of heart failure, which may result from perforation of a valve leaflet, rupture of chordae, blood flow obstruction due to vegetations, or intracardiac shunts from dehiscence of prosthetic valves, indicates a poor prognosis with medical therapy alone and a higher surgical risk (Braunwald et al. Valvular stenosis or regurgitation, myocardial damage, and mycotic (fungal) aneurysms are potential heart complications. Many other organ complications can result from septic or nonseptic emboli, immunologic responses, abscess of the spleen, mycotic aneurysms, and hemodynamic deterioration. A key strategy is primary prevention in high-risk patients (ie, those with rheumatic heart disease, mitral valve prolapse, or prosthetic heart valves). The objective of treatment is to eradicate the invading organism through adequate doses of an appropriate antimicrobial agent. Parenteral therapy is administered in doses that achieve a high serum concentration and for a significant duration to ensure eradication of the dormant bacteria within the dense vegetations. If the serum does not demonstrate bactericidal activity, increased dosages of the antibiotic are prescribed, or a different antibiotic is used. Numerous antimicrobial regimens are in use, but penicillin is usually the medication of choice. In fungal endocarditis, an antifungal agent, such as amphotericin B (Abelect, Amphocin, Fungizone), is the usual treatment. After adequate antimicrobial therapy is initiated, the infective organism usually disappears. The patient should begin to feel better, regain an appetite, and have less fatigue. During this time, patients require psychosocial support because, although they feel well, they may find themselves confined to the hospital or home with restrictive intravenous therapy. Surgical valve replacement greatly improves the prognosis for patients with severe symptoms from damaged heart valves. Aortic or mitral valve excision and replacement are required for patients who develop congestive heart failure despite adequate medical treatment, patients who have more than one serious systemic embolic episode, and patients with uncontrolled infection, recurrent infection, or fungal endocarditis. Many patients who have prosthetic valve endocarditis (ie, infected prostheses) require valve replacement.
Altered valve function can result from the enlarged stretched ventricle women's health clinic ucla purchase 1 mg arimidex with visa, usually resulting in regurgitation women's health clinic bankstown generic arimidex 1mg visa. Embolic events caused by ventricular and atrial thrombi as a result of the poor blood flow through the ventricle may also occur women's health center at huntington hospital generic arimidex 1 mg. The increased septal size may misalign the papillary muscles so that the septum and mitral valve obstruct the flow of blood from the left ventricle into the aorta during ventricular contraction pregnancy yoga poses arimidex 1 mg with amex. Structural changes may also result in a smaller than normal ventricular cavity and a higher velocity flow of blood out of the left ventricle into the aorta, which may be detected by echocardiography (Braunwald et al. Initially, only localized areas of the right ventricle are affected, but as the disease progresses, the entire heart is affected. Eventually, the right ventricle dilates and develops poor contractility, right ventricular wall abnormalities, and dysrhythmias. Examples of unclassified cardiomyopathies include fibroelastosis, noncompacted myocardium, systolic dysfunction with minimal dilation, and mitochondrial involvement (Richardson et al. Medical Management Medical management is directed toward determining and managing possible underlying or precipitating causes; correcting the heart failure with medications, a low-sodium diet, and an exerciserest regimen (see Chap. If patients exhibit signs and symptoms of congestion, their fluid intake may be limited to 2 liters each day. However, because of the limited number of organ donors, many patients die waiting for transplantation. The most common procedure is a myectomy (sometimes referred to as a myotomymyectomy), in which some of the heart tissue is excised. Septal tissue approximately 1 cm wide and deep is cut from the enlarged septum below the aortic valve. The length of septum removed depends on the degree of obstruction caused by the hypertrophied muscle. Instead of a septal myectomy, the surgeon may open the left ventricular outflow tract to the aortic valve by removing the mitral valve, chordae, and papillary muscles. The primary complication of both procedures is dysrhythmia; additional complications are postoperative surgical complications such as pain, ineffective airway clearance, deep vein thrombosis, risk for infection, and delayed surgical recovery. Since then, transplant procedures, equipment, and medications have continued to improve. Since 1983, when cyclosporine became available, heart transplantation has become a therapeutic option for patients with end-stage heart disease. Cardiomyopathy, ischemic heart disease, valvular disease, rejection of previously transplanted hearts, and congenital heart disease are the most common indications for transplantation (Becker & Petlin, 1999; Rourke et al. A typical candidate Clinical Manifestations the patient may have cardiomyopathy but remain stable and without symptoms for many years. Frequently, dilated and restrictive cardiomyopathy are first diagnosed when the patient presents with signs and symptoms of heart failure (eg, dyspnea on exertion, fatigue). Patients with cardiomyopathy may also report paroxysmal nocturnal dyspnea, cough (especially with exertion), and orthopnea, which may lead to a misdiagnosis of bronchitis or pneumonia. Other symptoms include fluid retention, peripheral edema, and nausea, which is caused by poor perfusion of the gastrointestinal system. The patient may experience chest pain, palpitations, dizziness, nausea, and syncope with exertion. Assessment and Diagnostic Findings Physical examination in the early stage may reveal tachycardia and extra heart sounds. With disease progression, examination also reveals signs and symptoms of heart failure (eg, crackles on pulmonary auscultation, jugular vein distention, pitting edema of dependent body parts, enlarged liver). Diagnosis is usually made from findings disclosed by the patient history and by ruling out other causes of heart failure, such as myocardial infarction. The echocardiogram is one of the most helpful diagnostic tools because the structure and function of the ventricles can be observed easily. Cardiac catheterization is sometimes used to rule out coronary artery disease as a causative factor. Chapter 29 Management of Patients With Structural, Infectious, and Inflammatory Cardiac Disorders 775 has severe symptoms uncontrolled by medical therapy, no other surgical options, and a prognosis of less than 12 months to live. A multidisciplinary team screens the candidate before recommending the transplantation procedure.