"Purchase crestor 20mg overnight delivery, cholesterol ratio the lower the better".
By: H. Ronar, M.A., M.D.
Medical Instructor, East Tennessee State University James H. Quillen College of Medicine
Rather cholesterol test diy order 5 mg crestor with mastercard, conservative cholesterol definition pdf cheap crestor 20mg on-line, nonimmunomodulatory therapy is appropriate for patients with these findings on kidney biopsy cholesterol ratio mmol/l purchase discount crestor. In this glomerulus cholesterol ratio 2.6 good discount crestor 20mg without prescription, many subendothelial "wire loops" and intracapillary "hyaline thrombi" are seen. Most patients with active proliferative lupus nephritis are treated initially with corticosteroids, traditionally a "pulse" of intravenous steroids (500-1000 mg/day of methylprednisolone for 3 days), followed by a high-dose oral regimen (usually prednisone at 1 mg/kg/ day, not exceeding 60 mg daily) that begins to taper at 8 weeks. Intravenous, compared to oral, cyclophosphamide therapy involves a lower cumulative exposure to drug, less frequent cytopenias, enhanced bladder protection, and fewer problems with adherence. Silver stain delineates the characteristic silver-positive spikes projecting from the glomerular basement membranes. Kidney biopsy evaluation is not complete without an assessment of both histologic activity and chronicity as a guide to therapy. Although this trial was largely performed in white subjects and may not be applicable to populations at high risk for poor kidney outcomes, reports from this trial with up to 10 years of follow-up continue to show no differences in outcome between treatment groups. The goals of continued immunosuppressive therapy are to prevent relapses and flares of disease activity, to eliminate smoldering activity leading to kidney scarring, and to minimize long-term side effects of therapy. Given the risk for long-term toxicities with all immunosuppressive agents as well as their potential effect on fertility and risk for teratogenicity, the selection and dosage of maintenance therapy are important and modifiable choices that doctors and patients should make together. Although no clinical studies exclude the use of steroids in maintenance therapy, many clinicians will discontinue steroids within the first 1 to 6 months of maintenance therapy to minimize side effects despite a lack of trial data for such a strategy. After at least 3 years of follow-up, both groups showed equal rates of remission, steroid withdrawal, and disease flares. Withdrawals resulting from severe adverse events were significantly more common among patients who were administered azathioprine. Intention-to-treat analysis showed a higher rate of complete remission and a lower incidence of adverse events with multitarget therapy at both 6 and 9 months than with cyclophosphamide-based induction therapy. Because of the unacceptably high rate of treatment failure (30% to 50%) of induction therapies, as well as the high rate of relapsing disease, newer agents and treatment strategies are continuously sought for lupus nephritis. Although more subjects in the rituximab group achieved complete or partial remission, there was no statistically significant difference in the primary clinical endpoint at 1 year. Other agents currently under study for treatment of lupus nephritis include belimumab, a humanized monoclonal antibody that targets the B cell growth factor B lymphocyte stimulator protein; abatacept, a selective T cell costimulation modulator; laquinimod, an oral immunodulatory therapy with an uncertain mechanism of action; and adrenocorticotropic hormone, which has proven effective in some cases of resistant nephrotic syndrome. In recent decades, the increasing armamentarium of immunosuppressive agents along with an improved knowledge, based on well-performed clinical trials, of how best to dose these agents has led to an improved prognosis for patients with lupus nephritis. Whereas kidney survival at 5 years was as low as 20% before 1980, current treatment strategies have improved this rate to as high as 80% in the past decade. Risk factors for progressive disease include demographic variables, such as male sex, African lineage, Hispanic ethnicity, low socioeconomic status, and young age at presentation, as well as clinical and biopsy features, such as higher serum creatinine at presentation, hypertension, anemia, percentage of glomeruli with necrosis or crescents, and degree of scarring or chronicity in the glomeruli and tubulointerstitium. When lupus nephritis does progress to end-stage renal disease, most patients experience a gradual complete or partial resolution of their extrarenal manifestations of lupus, including lupus serologies. Furthermore, those patients who continue to experience active disease generally have only mild to moderate symptoms. The mechanisms responsible for this apparent remission of systemic lupus in kidney failure remain unclear. Patients with end-stage renal disease due to lupus nephritis should be dialyzed for at least 3 to 6 months before kidney transplantation is performed; this recommendation holds particular importance for those patients with relatively rapid progression to kidney failure. This period allows for a potential further reduction in lupus activity before transplantation and affords patients with acute kidney injury sufficient time to recover kidney function if therapy is effective. Overall graft survival in patients with lupus who receive a kidney transplant is similar to those in patients with other kidney diseases, despite a recurrence rate of lupus nephritis that ranges from 5% to 30% depending on the indications for kidney allograft biopsy. Recurrence can occur as early as the first week to as late as 10 to 15 years after transplantation. Recurrent lupus nephritis does not necessarily follow the pattern of the native disease but often takes the form of a milder, nonproliferative lesion. Miyasaka N, Kawai S, Hashimoto H: Efficacy and safety of tacrolimus for lupus nephritis: a placebo-controlled double-blind multicenter study, Mod Rheumatol 19:606-615, 2009. The mortality rate of patients with diabetic nephropathy is high, with a marked increase in cardiovascular risk accounting for more than half of the increased mortality risk among these patients. Accordingly, there has been intensive research into early pathophysiologic mechanisms of diabetic kidney injury, predictors of risk for diabetic nephropathy, and early intervention strategies.
Gram-negative coccobacilli and polymorphonuclear leukocytes are commonly associated with Haemophilus influ enzae cholesterol hdl ratio normal value generic 5 mg crestor amex, which is a common cause of pneumonia in children cholesterol test dischem quality crestor 10 mg. This child suffers from a congenital diaphragmatic hernia caused by the failure of the diaphragm to properly form and close p-cholesterol-ratio order crestor 5mg with mastercard. The presence of bowel sounds in a lung zone indicates that abdominal contents have herniated past the boundary of the diaphragm into the thorax cholesterol test leeds cheap 5mg crestor overnight delivery. The developing diaphragm is derived from the Septum transversum, Pleuroperitoneal folds, Body wall, and Dorsal mesentery of the esophagus. These four components can be remembered by the mnemonic "Several Parts Build the Diaphragm. A continuous cardiac murmur (ie, present during both systole and diastole) could be the consequence of a patent ductus arteriosus, but is not related to the pleuroperitoneal folds and is unlikely to cause the presentation in this patient. Marked splenomegaly in children has many etiologies, but is unlikely to be consistent with the features of this vignette. Causes of splenomegaly include congenital infections and metabolic genetic disorders. These infections often cause hepatosplenomegaly, jaundice, mental retardation, and intrauterine growth retardation. Lysosomal storage diseases such as Gaucher disease, Niemann-Pick disease, Hunter syndrome, and Hurler syndrome also have symptoms of hepatosplenomegaly. Midline deviation of the trachea is commonly associated with pneumothorax or space-occupying lesions of the cervical region. Choice D represents the residual volume, which is the volume that remains in the lungs after a maximal expiration. Choice A represents the inspiratory reserve volume, which is the volume that can be inspired after inspiration of the tidal volume. Choice B represents the tidal volume, which is the volume inspired or expired with each normal breath. Choice C represents the expiratory reserve volume, which is the volume that can be expired after the expiration of the tidal volume. Choice E represents the inspiratory capacity, which is the sum of tidal volume and inspiratory reserve volume. It is the sum of the expiratory reserve volume and the residual volume, and it is the volume that remains in the lungs after a tidal volume is expired. Choice G represents vital capacity, which is the sum of tidal volume, inspiratory reserve volume, and expiratory reserve volume. This patient is showing signs of Cushing syndrome with a buffalo hump and purple striae. Of the different histological classifications of lung cancer listed above, small cell carcinoma is the most likely in the case for several reasons: Squamous cell and small cell carcinomas are most closely linked to smoking history (>98% are associated with smoking) and both present as central lesions such as that shown on the x-ray film. Adenocarcinoma is the most common lung cancer found in women and nonsmokers (although 75% are found in smokers). Adenocarcinomas are usually peripherally located, and are less likely to cause para-neoplastic conditions such as Cushing syndrome. Bronchial carcinoid is a rare neuroendocrine lung tumor that is not linked to smoking. These tumors cause cough, hemoptysis, and an increase the number of respiratory infections. Some of them are capable of producing serotonin and causes the classic "carcinoid syndrome" characterized by episodic attacks of diarrhea, flushing, and cyanosis. The picture shown here is that of a single solitary lesion, which is more likely to be a primary lung cancer. Squamous cell carcinoma accounts for 25%-40% of lung cancers and is closely linked to smoking. Like small cell carcinoma, squamous cell carcinoma also arises centrally and is associated with paraneoplastic syndromes.
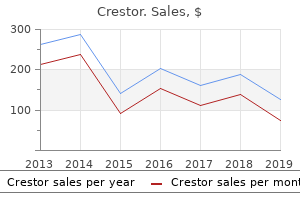
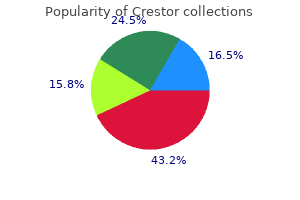
Discount crestor online. Portfolio Diet Challenge - Lowering Cholesterol Naturally.
A number of publications have highlighted the advantages of using the 30-20-10 "rule of thumb" for an orderly process of patient referral to a nephrologist and initiation of kidney replacement therapy is cholesterol in shrimp good for you generic crestor 10mg without prescription. It is essential to allay the anxiety and fear common in patients nearing kidney failure cholesterol medication taken off market cheap crestor generic. Whenever possible cholesterol medication in the news purchase crestor paypal, family members should be included in the decision-making process cholesterol ratio graph order crestor pills in toronto, and all members of the nephrology team, including the nephrologist, nurses, social workers, transplant coordinators, and dieticians, should participate in this process. If possible, patients and interested family members should visit the dialysis unit well before requiring dialysis, as this simple exercise may help alleviate many of their fears and misconceptions. Because most patients also anticipate much pain during dialysis, it should be stressed that almost no pain is involved. The need for compliance with diet, fluid intake, medications, and dialysis schedules should be stressed, and the patient should be empowered to participate in his or her own care, helping to ensure compliance and improve satisfaction. For patients presenting with an acute need to start dialysis, one option to consider is to frame dialysis initiation specifically as a trial, stressing that the decision to initiate is temporary and should not be binding. However, if a synthetic graft is all that is possible because of poor native vasculature, backup access is not recommended, because the risk-to-benefit ratio of synthetic grafts is unacceptably high in this situation. Although access should be planned first in the nondominant arm, sites should be preserved in the other arm as well. The use of the nondominant arm is preferred, particularly for self-dialysis, as it makes self-cannulation more likely. Radial arteries and cephalic veins should be preserved except in life-threatening situations. Whenever possible, phlebotomy should be limited to veins over the dorsum of the hand and the ulnar side of the forearm. If absolutely necessary, median antecubital veins may be punctured with small butterfly needles. In hospitalized patients, sites that are being preserved should be marked with a black felt-tipped pen as a reminder to all. For example, infants and children have high morbidity on long-term hemodialysis or peritoneal dialysis; accordingly, kidney transplantation offers the greatest likelihood of successful growth and development. On the other hand, morbidity and mortality for elderly patients may be higher with transplant than with dialysis, particularly in the absence of a living donor. The cause of kidney failure is an element that needs to be integrated into the selection of treatment options; for example, patients with brittle diabetes or previous abdominal surgery may benefit from thrice weekly in-center hemodialysis, whereas those with cirrhosis or severe cardiomyopathy may be treated more successfully with peritoneal dialysis or daily hemodialysis regimens. When multiple dialysis modalities are equally possible from a medical point of view, practical issues such as the presence of a supportive family environment, work habits, and economic factors. Vessels named are instrumental for the creation of hemodialysis fistula and grafts for vascular access. Upper-arm fistulas tend to have higher flow and therefore are more vulnerable to aneurysmal dilation; additionally, patients may have more difficulty self-cannulating upper-arm access. Access in Problem Patients In patients who cannot receive either a forearm or an upper-arm fistula using their own vasculature, a synthetic graft may be placed in the forearm. Either a distal radial artery to basilic vein (straight) graft or a loop from the brachial artery to the basilic vein should be considered. Synthetic grafts are more prone to infection and clotting than fistulas using endogenous vessels. Therefore, synthetic grafts should not be placed in anticipation of future dialysis need until generally 3 to 4 weeks before initiation of dialysis, with the recognition that optimal timing can be a challenge. Because of the much higher propensity for infections, catheter malfunction and inadequate blood flow through these catheters, and the risk of developing vein stenosis along the path of the catheter, it is critical that a permanent access plan be developed and implemented as soon as it is determined that the patient has chronic (and not acute) kidney failure. Finally, if the age and medical condition of the patient permit, living-related transplantation should be pursued. This section briefly discusses different dialysis techniques, including short daily hemodialysis and nocturnal hemodialysis, with a focus on conventional, thrice weekly, in-center dialysis, as this remains the most common hemodialysis strategy. The dialysis dose, the time needed to optimize kidney replacement therapy, and strategies for accomplishing this are reviewed. To place common hemodialysis strategies into context, current in-center hemodialysis regimens average less than 3. Considering that this level is below the level at which hemodialysis is initiated, it is clear that the delivery Because kidney disease is often "silent," it is inevitable that some patients will present with clear indications for initiation of dialysis but without a permanent access. Several factors should be considered in the prescription of dialysis to optimize outcomes. For the hypothetical 70-kg person, the first step is to calculate the volume of urea distribution, which is total body water.
With the new proposals cholesterol ratio verlagen generic 10mg crestor overnight delivery, concern remains that certain groups may be disproportionately disadvantaged cholesterol test how much blood buy crestor online from canada. As such cholesterol in shrimp bad crestor 5 mg discount, wait times have increased dramatically cholesterol medication starting with a discount 10mg crestor overnight delivery, to the point where it is difficult to accurately calculate median wait times in certain regions. Looking at it another way, only 30% of candidates will have received a kidney transplant within 3 years of being placed on the wait list. The lack of access to deceased donor organs, as well as the superior outcomes with live donors, has resulted in the increased usage of living kidney donors for transplantation. In the 15 years from 1990 to 2005, the number of living kidney donors used in the United States increased dramatically. Since 2005 this growth has slowed somewhat, but there were still more than 6500 living kidney donors used for transplantation in 2010 alone. Living kidney donation offers several potential advantages over deceased donor transplantation. First, the procedure is elective and scheduled, thus ensuring that both donor and recipient are in optimal medical condition. The planned nature of the operation also facilitates the use of preemptive transplantation. Second, the incidence of delayed graft function (need for dialysis in the first week posttransplantation) is much lower for recipients of living donor kidneys. Finally, patient and allograft survival rates are superior for living donor kidneys compared with deceased donors. In the most recently available data, patients who received a living donor kidney transplant in 2008 had a 1-year allograft survival of 96% compared with 92% for deceased donor recipients. For patients who received a living donor kidney transplant in 2004, the 5-year patient survival was 93% compared with only 85% for deceased donor recipients. Similarly, for those who received a living donor transplant in 2004, the 5-year allograft survival was 83% compared with only 70% for recipients of deceased donor kidney transplant. Many donors do, however, report benefits such as an improved sense of well-being from seeing a friend or relative thrive after transplantation. Given the exceptional circumstances surrounding living donation, it is crucial that informed consent be obtained in an open and thoughtful manner. Consent should be obtained for both the evaluation process and the surgical procedure itself. The potential donor needs to understand that the evaluation process requires a series of tests-and that the results of some of these tests may be abnormal. Other points that should be fully discussed as part of the informed consent process are outlined in Box 61. After informed consent, the evaluation consists of a psychosocial and medical assessment. The psychosocial assessment must be conducted by an appropriate professional Box 61. Living donor 9000 8000 Number of donors 7000 6000 5000 4000 3000 2000 1000 1990 1995 Deceased donor 2000 Year 2005 2010 Figure 61. This person will vary from site to site, but is most often a social worker, clinical psychologist, or psychiatrist. Significant concerns with any of these factors may preclude donation or require further assessment by other health care professionals. The medical assessment should be conducted by a surgeon or physician (ideally both) with expertise in living kidney donation. The goal of the medical evaluation is to determine (a) the overall health of the potential donor and whether he or she is fit for surgery; (b) the current kidney health of the potential donor and his or her risk for kidney disease or medical complications in the future; (c) the presence of any conditions that may result in disease transmission. The tests required to address these components of the medical evaluation are listed in Box 61. Before proceeding with specific testing, a medical history and physical examination is required for all living donors. The history should focus on conditions related to overall health and fitness for surgery, such as the presence of cardiovascular disease, liver disease, pulmonary disease, or hematologic conditions (bleeding disorders or thrombosis). Significant abnormalities in any of these areas may preclude donation or require more specialized testing and/or referral to another consultant. Most programs will not allow living donors younger than 18 years of age, and 15% of transplant centers require donors to be at least 21 years old. The most common upper age limit for living donors is 65 years old, and this cutoff was reported at 21% of American transplant centers in a 2007 survey.