"Order genuine lynoral on-line, oxygenating treatment".
By: F. Bufford, M.A., M.D., Ph.D.
Co-Director, Case Western Reserve University School of Medicine
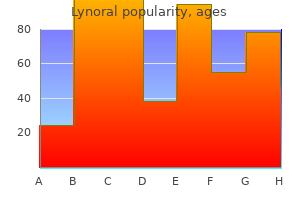
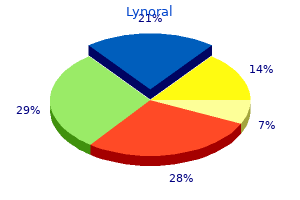
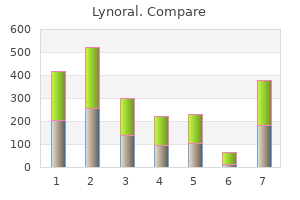
Congenital Abnormalities of the Trachea Tracheomalacia Tracheomalacia is an abnormal collapse of the trachea due to localized or generalized weakness of the tracheal wall (Fig medicine 5113 v lynoral 0.05mg with amex. In primary tracheomalacia crohns medications 6mp discount lynoral 0.05 mg otc, there is an intrinsic abnormality of the tracheal wall medicine for high blood pressure generic 0.05mg lynoral with amex, whereas in secondary cases there is extrinsic compression treatment ingrown toenail buy lynoral 0.05mg free shipping. In congenital cases, this is usually in association with cardiovascular abnormalities including the following (discussed in more detail later in the chapter): 1. Pulmonary artery sling-compresses the right main bronchus Congenital tracheomalacia may be associated with bronchomalacia, particularly in more generalized cases. The clinical manifestations of the condition are very variable, and it is often a diagnosis that can only be reliably made by endoscopy. There is likely to be stridor, which is usually expiratory as the obstruction is predominantly intrathoracic. There are usually recurrent acute episodes of stridor and dyspnea, during which the child may become cyanosed and moribund ("dying spells"). The symptoms are usually apparent in the immediate neonatal period but may deteriorate in the first and second year of life, in an almost stepwise manner. The pediatric airway is very elastic and may collapse during forceful inspiration and certainly during coughing fits. The membranous part of the trachea also tends to bulge forward, giving the impression of a narrow airway. During endoscopy, it is important that the child is adequately anesthetized to avoid coughing while there is still spontaneous respiration. There is no generally accepted definition of the degree of collapse that can be taken as abnormal, but it seems reasonable to suggest that more than 25% reduction of the lumen is a significant finding and that greater than 50% is likely to be symptomatic. As well as overdiagnosis, it is possible to miss the condition if the trachea is splinted by the bronchoscope or if there is excessive positive end-expiratory 334 Respiratory Disorders in the Newborn pressure applied by the anesthetist through the sidearm of the instrument. There may be associated recurrent respiratory infections, and training in home chest physiotherapy may need to be provided. In more severe cases, active treatment might be considered, though many of the choices have severe potential complications and should only be utilized in the face of extreme circumstances: 1. This may relieve the compression though once the tracheal wall has become weakened from external pulsatile pressure, it may not immediately recover following removal of the anomalous vessel. A suture through the adventitial lining of the aortic arch and the periostium of the sternum is used to pull the arch forward. As the anterior tracheal wall is intimately connected to the aortic arch with fascial tissue, it is also towed forward, thus widening the tracheal lumen. There may be a failure of the suture, and there is a risk of damage to the aortic arch itself. This procedure can be performed via a thorascopic approach, which has the potential of reducing operative morbidity. This is very effective for short-segment tracheomalacia but is unsatisfactory when the distal trachea is involved. The tube tip has to pass through the segment to stent it; custom-made tubes can be manufactured to optimize the length. However with a distal segment, the tube tip may pass into the right main bronchus on neck flexion and may not adequately stent the tracheomalacic segment on neck extension. These are typically made from siliconized plastic or are designed as expandable metal tubes. Stents may be highly effective at maintaining the lumen of the trachea but can be difficult to introduce down a bronchoscope and may be complicated by displacement, granulation tissue, and infection. Rib cartilage grafts can be used to stiffen the tracheal wall, but if near to half of the tracheal wall is replaced there can be slow or incomplete re-epithelialization. Congenital Tracheal Stenosis (Complete Tracheal Rings) In this very rare condition, there is a segment of the trachea, often distal, where the tracheal rings are truly complete. It is often found in combination with other regional abnormalities, particularly cardiac, including pulmonary artery sling. Alternatively, the child may suffer immediate respiratory distress in the delivery room that is not relieved by intubation or even tracheostomy. Extracorporeal oxygenation may be necessary to allow time to consider a surgical remedy. If the child is relatively stable, it may not be necessary to consider any form of tracheal surgery, and there is potential for airway growth with the child.
Castorbean (Castor). Lynoral.
- Stimulating full-term labor in pregnant women.
- Constipation.
- Are there any interactions with medications?
- What other names is Castor known by?
- What is Castor?
- Syphilis; arthritis; skin disorders; boils; blisters; swelling (inflammation) of the middle ear; migraines; softening cysts, warts, bunions and corns; promoting the flow of breast milk; and other conditions.
- Dosing considerations for Castor.
- How does Castor work?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96863
Regardless of the age of the patient and the underlying cause of pneumothorax symptoms zyrtec overdose discount lynoral 0.05 mg online, massive or continued air leak elevates the intrapleural pressure to above atmospheric pressure symptoms uterine prolapse buy lynoral, a condition known as tension pneumothorax treatment concussion purchase genuine lynoral line. The ipsilateral lung collapses because its elastic recoil can no longer be counteracted by the outward pull of a previously subatmospheric pleural pressure symptoms ptsd generic lynoral 0.05mg otc. The contralateral lung is overexpanded during inspiration, and, as a result, greater retractive force develops, pulling the mediastinum toward it during expiration and impeding venous return to the heart. Because ventilation is impaired, greater inspiratory efforts develop in an attempt to generate sufficient negative pleural pressure to ventilate the normal lung, aggravating the tension pneumothorax, shifting the mediastinum further, and severely impeding systemic venous return to the heart. Compensatory tachycardia occurs and further decreases diastolic filling and ventricular output, with cardiac standstill imminent unless the pulmonary tamponade is decompressed. Lung collapse per se does not contribute in a major way to poor gas exchange because there is redistribution of pulmonary blood flow to the normal lung, which will have lower vascular resistance. Chest radiograph of a neonate with hyaline membrane disease, demonstrating pneumomediastinum (straight arrow), massive subcutaneous emphysema, and pneumoperitoneum that is pushing the liver down (curved arrows). Furthermore, abnormality of the pulmonary parenchyma, as with sarcoidosis, histiocytosis, or interstitial lung disease predisposes to secondary pneumothorax. Airway abnormalities with resultant overdistension of peripheral pulmonary parenchyma, as with asthma, cystic fibrosis, emphysema, or mucoid impaction of the airway may result in lung rupture. A, Posteroanterior chest radiograph demonstrating a spontaneous left tension pneumothorax, with a shift of the cardiac silhouette and the mediastinum to the right. B, Posteroanterior chest radiograph after insertion of a chest tube on the left shows a residual moderately sized pneumothorax. Chronic lung disease that decreases lung elastic recoil and concomitant pleural adhesions prevents total collapse. A patient may have sudden cardiorespiratory collapse without clinical warning or antecedent roentgenographic changes, or he or she may be asymptomatic, with the diagnosis made initially on the basis of chest roentgenogram. Early recognition of lung rupture requires keen awareness of its possibility, particularly in patients with conditions known to be associated with this complication (Box 70-4). Pneumothorax may also be a spontaneous event, unrelated to any known cause, particularly in newborn infants and tall, lean adolescents and young adults. In an otherwise normal neonate, symptoms of spontaneous pneumothorax are often subtle, and physical findings are misleading because abnormalities may not be immediately discernible. Certain clinical features, however, have been seen on close observation: (1) the infant is unusually irritable; (2) tachypnea with a respiratory rate >60 breaths/min is invariably seen; and (3) chest bulging is usually noticeable, especially with unilateral pneumothorax. A shift of the cardiac impulse away from the site of pneumothorax is a useful sign, but often it cannot be detected confidently. It is also difficult to identify diminished air entry on the ipsilateral side because of the small size of the newborn chest. Grunting, retraction, and cyanosis are noted late in the progression of the complication. In a newborn with underlying lung disease requiring mechanical respiratory assistance, certain observations are useful to note. Sudden deterioration, accompanied by decreased compliance of the respiratory system and the need for increased inspiratory pressure, suggests a diagnosis of tension pneumothorax, which necessitates prompt needle decompression. Changes in vital signs include decreases in heart rate, blood pressure, and respiratory rate, and narrowing of pulse pressure. Even when deterioration is gradual, auscultation is often unreliable because breath sounds from the remaining expansible Air and Liquid in the Pleural Space areas of the lungs are clearly transmitted across the small newborn chest during mechanical ventilation. Although certain limitations of physical examination of the chest have been alluded to , periodic physical reappraisal remains important and must be done whenever a patient shows clinical worsening, deterioration in arterial gas tensions, or both. Additional nonroentgenographic tools for monitoring infants for pneumothorax in highrisk situations. In neonates, chest transillumination with a powerful fiberoptic light probe has been effectively applied to the diagnosis of pneumothorax at the bedside and has a distinct advantage. These techniques allow for more focused use of the chest radiograph in following these neonates. Roentgenographic confirmation is essential when the physical findings are minimal and cardiorespiratory function is only modestly altered.
Certain pharmacologic agents can cause apnea xerostomia medications side effects buy 0.05mg lynoral with mastercard, including barbiturates and sedatives medications used to treat bipolar order lynoral online from canada. Additional treatment is required if the apneas are frequent or severe or are associated with prolonged desaturation medications rheumatoid arthritis purchase lynoral 0.05 mg with amex. Treatment with methylxanthines symptoms pneumonia purchase generic lynoral online, theophylline, and caffeine reduces apnea in preterm infants. Caffeine is the preferred agent because oncea-day dosing is possible due to its longer half-life, and it has a higher therapeutic index than theophylline. Side effects of theophylline include hyperactivity, tachycardia, cardiac dysrhythmias, feeding intolerance, and seizures. The frequency of apnea is decreased by increasing the functional residual capacity, stabilizing oxygenation, and/or by splinting the upper airway. Infants with severe and refractory apnea may need to be intubated and supported by mechanical ventilation; minimal ventilator settings should be used to reduce the risk of volutrauma. Apnea preceded by a fall in pH to less than 4, recorded by a probe placed in the esophagus, is diagnostic of reflux-stimulated apnea. Although pH monitoring is often considered the standard diagnostic test, its use is limited in preterm infants, as their gastric pH is >4 for 90% of the time. Impedance testing, which will detect non-acid reflux, is an alternative, but there is no evidence that non-acid reflux causes symptoms or reflux disease. If the symptoms persist, "thickeners" should be given or nasojejunal feeding instituted. In the presence of gastric acid, alginates precipitate forming a gel that floats on the surface of the gastric contents and provides a relative neutral barrier; Gaviscon (sodium alginate) can increase the sodium content of feed, which may be undesirable in very prematurely born infants. Erythromycin binds to motilin receptors and stimulates gastric antral contractions and induces antral migrating motor complexes, which are important for gastric emptying. Treatment with erythomycin was associated with more positive effects in improving feeding intolerance when a higher dose (40-50 mg/kg/day) was used or the treated infants were 32 weeks gestational age or older. Hyaline membranes line the terminal airways, hence the alternative name of hyaline membrane disease. Poor clearing of lung fluid, inadequate respiratory efforts, and underdeveloped chest wall and respiratory muscles compound the infants problems. They differentiate from the columnar epithelium during the canalicular phase of development but are not prominent until about 24 weeks of gestation. Surfactant is a complex mixture of substances including phospholipids, neutral lipids, and proteins. Lipids are the major constituent of surfactant; the most important are phosphatidylcholine and phosphatidylglycerol, representing 70% to 80% and 5% to 10% of the lipids respectively. Phosphatidylinositol, phosphatidylserine, and phosphatidylethanolamine make up a further 10% of the lipids in surfactant. About 10% of the total lipids in surfactant are neutral lipids: cholesterol, triacylglycerols, and free fatty acid. Surfactant is synthesized in the endoplasmic reticulum; the phospholipid then moves via intracellular pathways to the lamellar bodies, which unravel to highly surface active tubular myelin. There is direct transition from the tubular myelin to the surface film, with absorption of a mixture of saturated and unsaturated phospholipids. The surface film is then refined by selectively squeezing out unsaturated phospholipids, generating small vesicular forms of surfactant, which have poor surfactant activity. The loss of surfactant into the airways is proportional to the rate and depth of respiration and can be reduced by addition of continuous positive airway pressure. Surfactant lost in this way is swallowed or, in fetal life, moves into the amniotic fluid. Surfactant may be degraded locally in the alveoli and small airways, the breakdown products being absorbed and recycled by the alveolar cells. More than 90% of the phosphatidylcholine on the alveolar surface is reprocessed, the turnover time being approximately 10 hours. Surfactant secretion is controlled by stretch receptors and stimulated by alveolar distension.
In the same way as pediatricians recognize that it is inappropriate for adult-trained physicians to manage young children medications list a-z discount 0.05 mg lynoral fast delivery, it also becomes increasingly inappropriate for pediatricians to continue to care for their patients once they have completed the tasks of adolescence and are living their lives as adults symptoms yellow fever order lynoral mastercard. While pediatricians may feel relatively confident and competent managing certain disease-specific aspects of respiratory disorders such as asthma or bronchiectasis medications 2355 generic 0.05 mg lynoral fast delivery, more general areas of adult health care medicine 3605 generic lynoral 0.05mg without a prescription. However, in the interest of optimal health care, it is important that whatever model is employed, professionals who manage adults with chronic respiratory disease receive adequate training in general adult health issues. It is widely acknowledged that this is a continuous process leading to the single event of transfer of care. While there are certain elements of transition that are diseasespecific, there are many aspects that are generic to all chronic illness. Russell Viner, a leading advocate for Differences Between Pediatric and Adult Models of Care Logistical and financial considerations also come into play when considering transition. Some suggest making transition a topic of discussion from the moment of diagnosis. In practice, this may prove difficult, given the amount of information that families have to take in at the time of diagnosis of a chronic illness. However, the prospect of transition to adult care is an issue that needs to be brought up in any discussion of long-term prognosis-a subject that usually arises in conversations at an early stage. For older children and adolescents, there is no "right" time to start increasing the focus on transition. However, the consensus is that the emphasis on transition should increase as children enter adolescence, often at the same time as they move from primary to secondary school. Transition is one aspect of the wider process of providing developmentally appropriate health care for adolescents. Health professionals can employ certain practical strategies to help promote healthy adolescent development and prepare adolescents for their subsequent move to adult care. These strategies include the following: · Seeing adolescents on their own, separate from their parents, for part of the consultation · Emphasizingtheimportanceofconfidentiality · Discussing understanding of their illness and actively promoting self-management · Addressinggeneraladolescenthealthissues,inaddition to those related to their specific condition Seeing adolescents alone for part of the consultation is a visible way of demonstrating to them and their families that adolescence is a time of developing independence. It conveys a message to the whole family that it is appropriate for the adolescent to begin to take increasing responsibility for his or her own health. Asking questions about school, friends, and activities shows an interest in the adolescent as an individual, rather than his or her disease. These have the dual purpose of gathering information and allowing time to develop rapport. As discussed later in the chapter, mental health problems and health risk behaviors such as smoking, alcohol and other drug use are common in adolescents with chronic illness and always need to be considered. The disclosure of any activity that puts the young person at serious risk of significant harm (such as suicidal thoughts or physical/sexual abuse) cannot remain confidential. If adolescents are assured of some degree of confidentiality, they are more likely to speak frankly. Pediatricians can assist in helping adolescents to develop self-management skills through the gradual process of increasing the focus on the adolescent, rather than their parents, during each consultation. As mentioned earlier in the chapter, this is helped by seeing adolescents on their own. Discussions should focus on the understanding of their illness, their priorities and goals, the reasons for and the effects of adhering to a specific treatment regimen, and ways to minimize the impact of the illness on their day-to-day life. These include how to book or reschedule an appointment, obtaining prescriptions and knowledge of any fees payable, whom to contact in an emergency, and how to get to the adult clinic. These are issues common to all chronic illnesses, and when addressed can help to reduce the anxiety around the eventual transfer of care to an adult center. An example is shown in Table 16-4, and others are available on the transition websites listed in the Suggested Reading at the end of the chapter. In support of this approach, a recent study in primary care involving adolescents 11 to 16 years of age demonstrated that adolescents had more positive perceptions of their primary care physician when sensitive issues such as drugs, sex and mental health were discussed. However, taking a long-term view, the argument for providing intensive input during adolescence and young adulthood is that this will lead to improved health outcomes and reduce the potential for unscheduled emergency visits and hospital admissions, which account for the majority of the health care costs associated with chronic illness. Providing an environment where patients can be seen alone in suitable physical surroundings. Simple measures can be very effective, such as considering the color scheme of the clinic area, the furniture, and the reading material available. The participation of young people in the design of clinical areas is extremely valuable and is likely to increase the chances of their remaining engaged in their own health care. For cystic fibrosis, the existence of specialist adult centers is well established, and the models of transition are those to which other subspecialties often look for guidance.
Order 0.05mg lynoral with visa. Depression; Feeling Depressed - Anxiety Symptoms.